Apr 2, 2013
First of all I would like to make it clear that what you are about to read is largely driven by my own opinions based on what I have read, and what I have seen in my years both as an EMT and a paramedic. With enough research though, I feel confident that I could present a substantial amount of “facts” to back this up.
Response times DO NOT improve ROSC rates.
Directly.
In article after article about response times, there is always that little asterisk that says “in MOST cases response times do not matter.” Well, I am going to go as far to say that in ALL cases response times do not matter. There are far more important things than response times in providing a high quality Emergency Medical Service. I say specifically Emergency Medical Service because Skip Kirkwood made a terrific point in his comment in a recent blog post: “(An) ‘ambulance service’ is not the same thing as ‘EMS.’”
Now, let’s just suppose for a second that we go with the common statement that response times improve outcomes. An ambulance pulls out of their station or away from their street corner and goes flying across a city, or through suburbia, lights and sirens blaring, and they pull up in front of the address of a patient in cardiac arrest. Then what? If that ambulance makes it there in 8 minutes and 59 seconds or less, do the EMS gods simply smile, say “job well done!” and your patient is magically resuscitated? No. Far more goes into it than that.
So if response times do not improve ROSC rates, what does make a difference? Well, let’s start from the beginning:
1. Public CPR education – Seattle has proven that when trained, people are willing to help. The rest of the country should follow their example and push public education. That does not exactly mean putting a CPR card in the back pocket of every citizen, it might just mean educating them on the importance of compressions only CPR.
2. Public access AED’s – Again, here is another piece in the pie that rests mainly on the public. Since I have been traveling more for conferences I have always kept an eye out in almost every major airport I’ve been to, looking for AED’s to see how accessible they are to the public. For the most part, I have been pretty impressed. I recently joined a new gym, and one of the main features that I was looking for that was in plain view of the entire gym was an AED hanging on the wall right under the “emergency phone.”
On the other hand though, I do not feel that I see nearly enough publically accessible AED’s in malls and store fronts that I have shopped in.
3. A highly trained dispatch center – When tragedy happens and someone picks up their phone and calls 9-1-1, the person at the other end needs to be ready for anything, and they need to be calm, cool, and collected as they give pre-arrival instructions. Because such a large portion of the population is not trained in CPR, someone needs to talk them through the process.
4. A highly trained workforce staffing ambulances – It does not matter if they are fire based, private, municipal, volunteer, or any other model that you can possibly think of. The important thing is the EMTs and paramedics who respond need to be trained and up to date. They also have to be willing and ready to embrace the nuances of the recent advancements in pre-hospital cardiac arrest and post cardiac arrest care: minimize interruptions in compressions, and stress the importance of compressions.
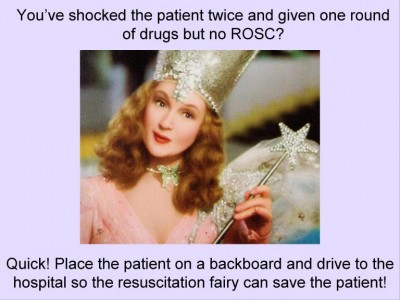
5. Don’t transport! – Last but certainly not least, a patient has to be worked where they “drop.” About a month ago, Tom Bouthillet from EMS12Lead.com created a Meme, an internet cartoon for me, that while it made me laugh was the perfect depiction of cardiac arrest care in my last system: it is a picture of Glinda, the Good Witch of the North from The Wizard of Oz with the caption, “You’ve shocked the patient twice and given one round of drugs but no ROSC? Quick! Place the patient on a backboard and drive to the hospital so the resuscitation fairy can save the patient!”
The worst thing you can do for a person in cardiac arrest, and especially V-Fib or V-Tach is to throw them on a backboard and rush them to the hospital. The most important time in cardiac arrest care is those first ten or fifteen minutes. That is not only the time where we are most likely to save someone, but if we do save them that is when those patients are most likely to have the best outcomes.
It is time for communities to stop high fiving themselves for fast response times. It is time for state organizations and offices of EMS to recognize what is important, and stop acting as “offices of ambulance response.” As long as city council members and TV stations raise concerns about “long response times” then our EMS systems will not live up to the expectations that we as an industry place on them.
I am going to quote Skip Kirkwood again, who was quoting Frank Stroud: “ambulance services can be fast, cheap, or efficient. Choose two out of the three.”
So who tells everyone? Who leads the charge and dares to educate the public about what really happens in the back of an ambulance? That is a question that I do not know the answer to. What we need to do though is get over our fear of HIPAA laws, and with that, get over our fear of the media. We need to dare to point out where we as an individual system and industry can improve. And we need to stop hanging our hats on what we feel that everyone else thinks is important: the ability to throw on those lights and sirens, and give that call a good old fashioned diesel bolus.
Those days are over. We need to realize it and admit it and then help everyone else do the same. Let’s get rid of the smoke and mirrors.
You know what? On second thought maybe that response time asterisk should stay. But it should say “Response times matter when the unit responding is delivering responders trained in high quality CPR.” That is a statement I could get behind.



Scottie… No truer words have been spoken… In my short time in EMS (3 decades or so), I have seen too many EMS accidents because of inappropriate speed, in fact even lost a good friend, Leslie Gocek to inappropriate EMS driving. There is much wisdom in the EMS Garage podcast #153 Ghost of Christmas Past… The panel addressed one of the most important issues and that’s changing EMS to a culture of safety. I know that I currently serve on the NJ OEMS Safety Committee and this is our objective. Community CPR in monumental and how about better EMS CPR… the new standards are more physcially demanding but it works! Community outreach is paramount to our survival. Teach the young the old and everyone inbetween so they can be part of our system. Mandate EMD nationwide and the practice of CPR prior to a first responder arriving. Quickly teach the caller to be the first responder. Now these practicies takes the bullet out of the gun for those who advocate driving a 15k gvw weapon like a bat out of hell… Practice good medicine and good EMS… So we just don’t educate the masses on various levels to perform quality CPR, but we educate the politicians to the fact that 8:59 (or whatever your contract’s dictate) is not an acceptable or prudent practice, we educate our staff to the dangers of getting clearance from your local Air Traffic Control and define our expectations of them, we mandate change in our dispatch systems and when all else falls…. buy a LUCAS II Device for every patrol car and downgrade to a Charlie Response to reduce liabiltiy exposure… Now we can safely address ROSC…
Uncle Joey
Well said Scottie. I cheerfully and emphatically linked to this on my fbook page. I echo Mr. Rubba’s comments as I attended Leslie Gocek’s funeral and bring her story up in almost every class I teach or every discussion about safety, response times etc… that I partake in.
The absolute obsession with “out of chute” and “response times” (always with the attached “but safely” nonsense) has driven me up a wall with some. I find it myopic and unrealistic at best and an outright disregard for my personal safety and ability to sustain my family at worst.
Thank you for so eloquently putting in words what most medics have been saying for years. Having been an EMS Educator in a past life, I always told both BLS and ALS that the more serious the condition of the patient, the more slowly the transport should be done. One of my pet peeves is when Police, Fire, Dispatch, or EMS units ask you to expedite. Really! We are going as safely and quickly as possible. Don’t panic, we will get there or meet you en-route! 🙂